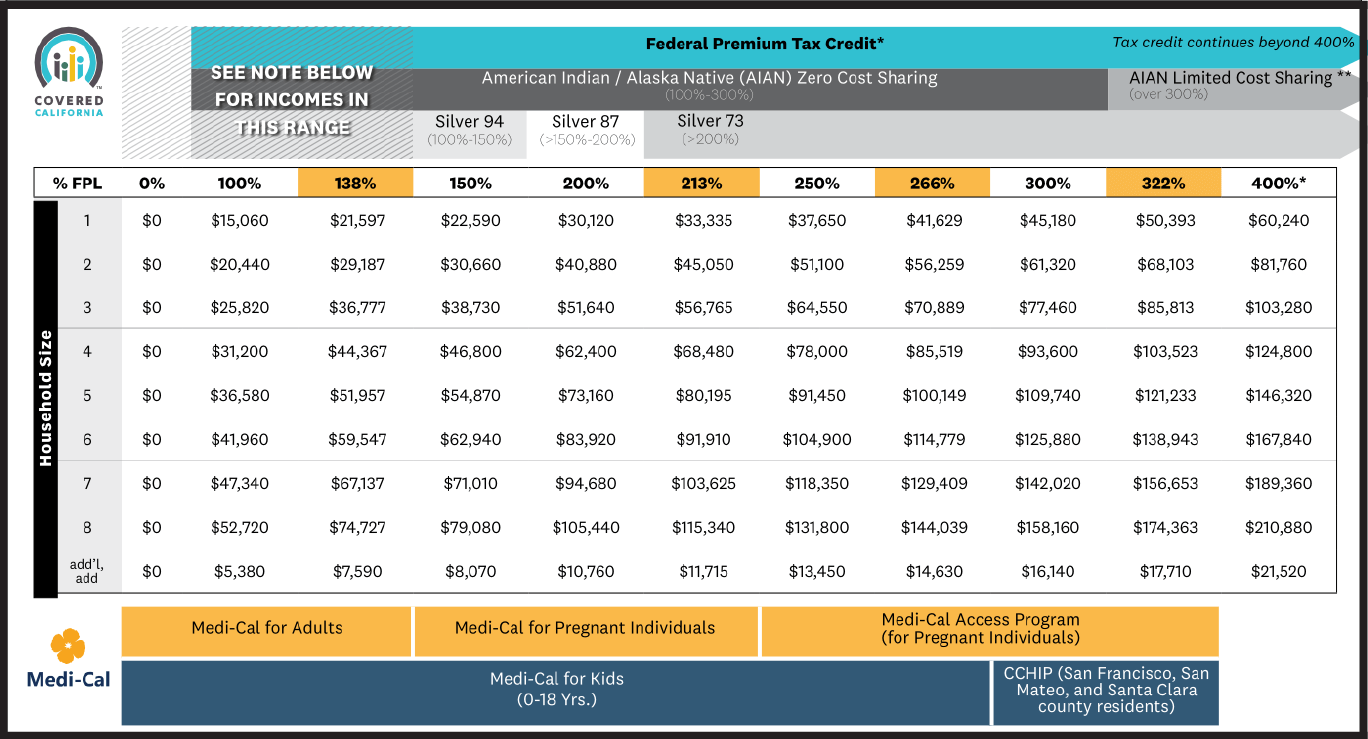
The Covered California income limits require consumers to have a household income that ranges from 0% to 400% of the Federal Poverty Level (FPL) in order to qualify for assistance on a government health insurance plan. See the Covered California 2024 income limits chart below.
Your financial help and whether you qualify for various Covered California or Medi-Cal programs depends on your income, based on the Federal Poverty Level (FPL).
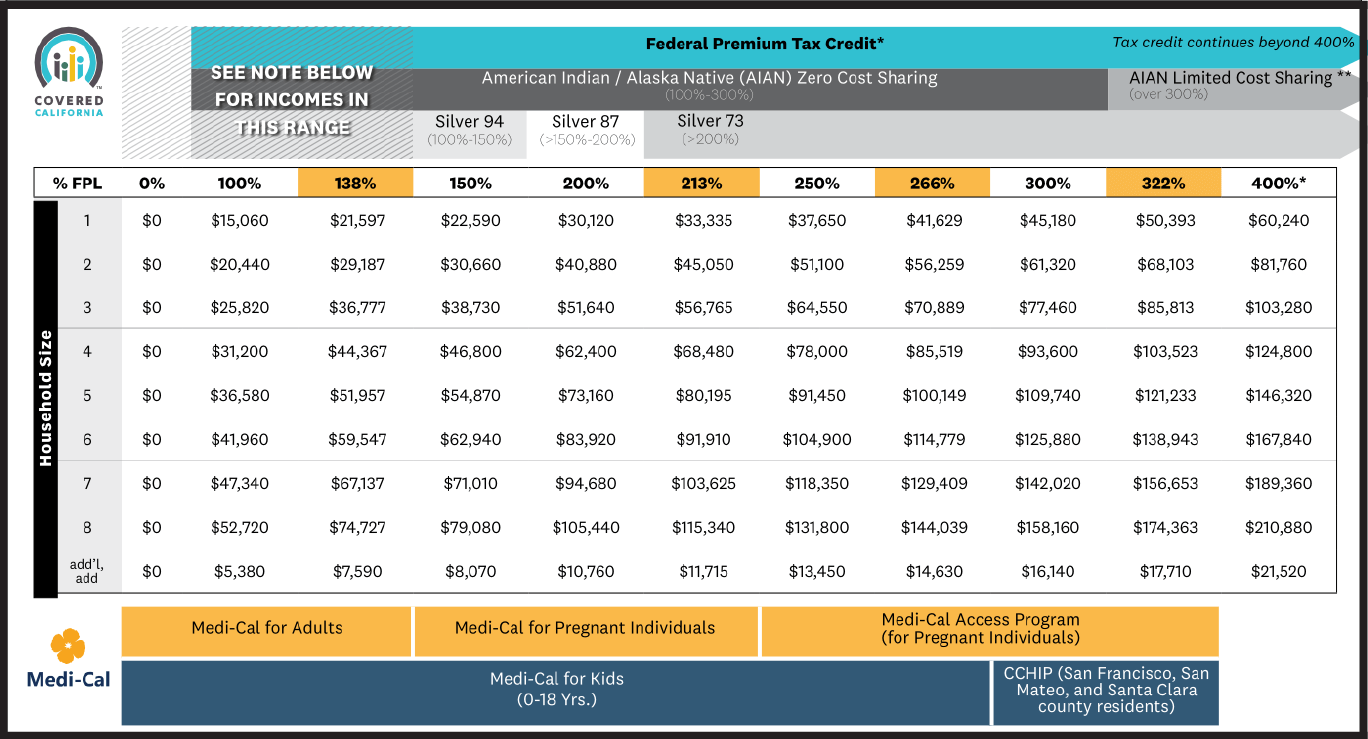
* Consumers at 400% FPL or higher may receive a federal premium tax credit to lower their premium to a maximum of 8.5 percent of their income based on the second-lowest-cost Silver plan in their area.
Based on your household income, you may qualify for up-front tax credits when you enroll in health insurance in California through the Covered California Health Exchange. Be aware that free health insurance plans are available!
According to Covered California income guidelines and salary restrictions , if an individual makes less than $47,520 per year or if a family of four earns wages less than $97,200 per year, then they qualify for government assistance based on their income. If the family has a lower household net income, then a greater amount of government assistance is available to the family. Tax deductions can lower your income level. View the Covered California income limits chart below.
Under the Affordable Care Act, all marketplace and Medicaid plans need to provide coverage for pregnancy and childbirth. You qualify for pregnancy coverage even if you’re already pregnant when you apply for coverage. It’s important to have health coverage when you’re planning on having a baby for the following reasons:

Since having health coverage and getting access to healthcare is critical during pregnancy, the income requirements for pregnant people are slightly different than those for people who aren’t currently expecting a baby. Here’s what you might qualify for, depending on your income level:
When you apply for Medi-Cal while pregnant, your eligibility is presumed while your application is reviewed. That means you can take advantage of immediate coverage, ensuring you and your baby get the care you need.
Adults qualify for Medi-Cal with a household income of less than 138% of FPL. However, according to the Covered California income guide, children who enroll on Obama Care California plans may qualify for Medi-Cal when the family has a household income of 266% or less. The children must be under 19 years of age to qualify. Also, C-CHIP, the County Children’s Health Initiative Program, offers health care coverage for children when the family income is greater than 266% and up to 322% of FPL.
Document proofs (including pay stubs, bank statements, etc.) may be required to verify your household income threshold. If you fail to provide proof of income, you may lose your Obamacare subsidy or your health care coverage.
Acceptable proof can include:
If your income increases during the year, this may affect what levels of subsidies you qualify for according to Covered California income limits. It also may affect whether or not you, your spouse or your children qualify for certain government assistance programs. If you have a significant income change mid-year, you may be required to report that to Covered California or to Medi-Cal.
If you need health insurance or help affording health coverage, you might qualify for Medi-Cal or a subsidy. Health for California can help you determine whether you qualify for a subsidized or Medi-Cal plan based on your income and current situation. Get a quote today.